Rn comfort rest and sleep assessment – Delving into the realm of RN Comfort, Rest, and Sleep Assessment, this comprehensive guide provides a profound exploration of its significance, assessment methods, influencing factors, nursing interventions, patient education, documentation, and future directions. Prepare to embark on a journey that unravels the intricacies of patient well-being and empowers nurses with the knowledge and skills to promote optimal comfort, rest, and sleep outcomes.
RN Comfort, Rest, and Sleep Assessment: Introduction: Rn Comfort Rest And Sleep Assessment

Assessing comfort, rest, and sleep is crucial for patients’ well-being and recovery. Inadequate comfort, rest, and sleep can lead to impaired physical and cognitive function, delayed healing, increased risk of complications, and decreased patient satisfaction.
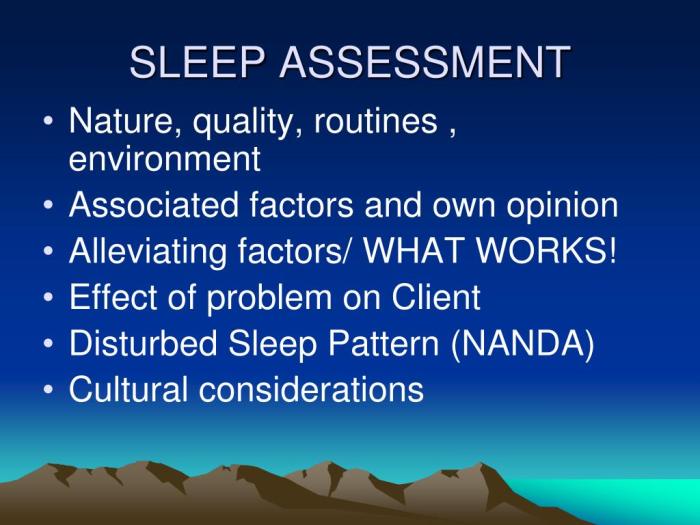
Nurses play a vital role in assessing and managing patient comfort, rest, and sleep through various methods, including scales, questionnaires, and observation.
Assessment Methods
- Numeric Rating Scales (NRS):Patients rate their comfort level on a scale of 0-10, with 0 indicating no discomfort and 10 indicating extreme discomfort.
- Visual Analogue Scales (VAS):Patients mark a line to indicate their comfort level on a continuous scale, typically ranging from “no discomfort” to “worst possible discomfort.”
- Comfort Assessment Tool (CAT):A comprehensive tool that assesses multiple dimensions of comfort, including physical, psychological, and environmental factors.
- Rest Assessment Instrument (RAI):A structured interview that assesses sleep quality, duration, and daytime sleepiness.
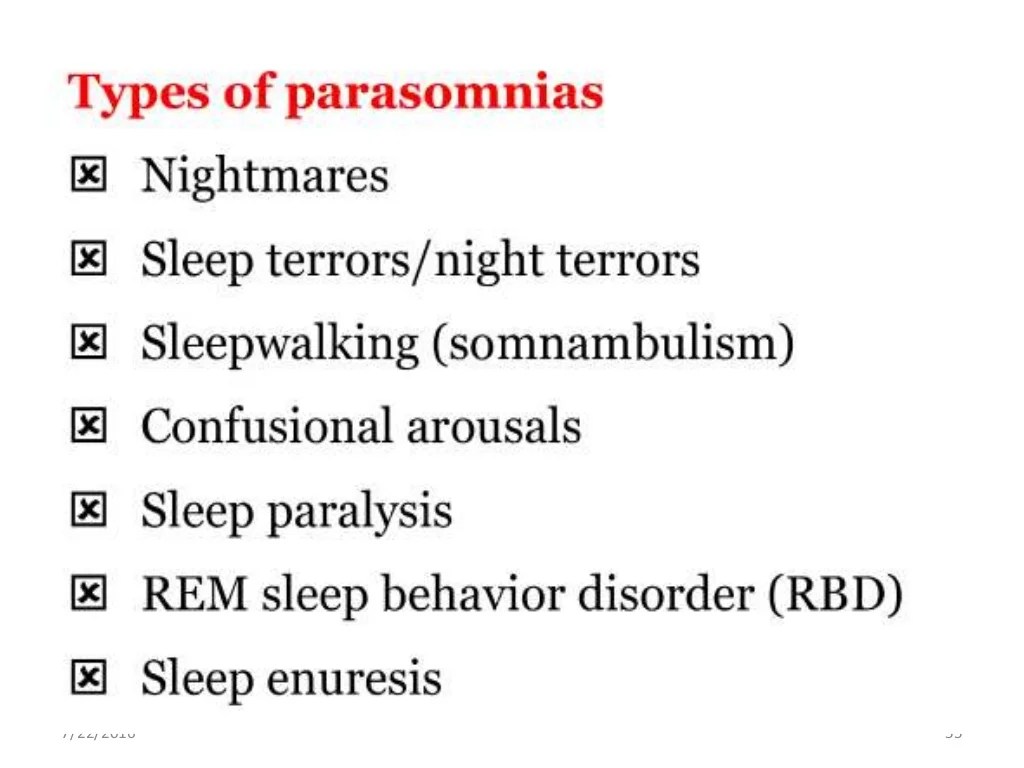
Factors Influencing Comfort, Rest, and Sleep, Rn comfort rest and sleep assessment
Physiological Factors
- Pain
- Fatigue
- Nausea and vomiting
- Respiratory distress
Psychological Factors
- Anxiety
- Depression
- Stress
- Cognitive impairment
Environmental Factors
- Noise
- Light
- Temperature
- Comfort of the bed and bedding
Social Factors
- Social support
- Privacy
- Cultural beliefs and practices
Nursing Interventions
- Managing Pain:Administering pain medication, providing non-pharmacological pain relief measures (e.g., massage, heat/cold therapy).
- Reducing Anxiety:Providing reassurance, teaching relaxation techniques, administering anti-anxiety medication if indicated.
- Optimizing Environment:Controlling noise, light, and temperature; providing comfortable bedding.
- Promoting Restful Sleep:Establishing regular sleep-wake cycles, creating a conducive sleep environment, avoiding caffeine and alcohol before bedtime.
Patient Education
Educating patients about sleep hygiene, relaxation techniques, and other self-care measures is essential for promoting comfort, rest, and sleep. Nurses can provide written materials, conduct group sessions, or offer one-on-one counseling.
Documentation and Evaluation
Accurate documentation is crucial for tracking patient comfort, rest, and sleep and evaluating the effectiveness of interventions. Nurses should record assessment findings, interventions implemented, and patient responses.
Evaluation involves monitoring patient outcomes, such as improved comfort levels, increased sleep duration, and reduced anxiety.
Case Study or Example
A 55-year-old patient with a hip fracture is admitted to the hospital. The nurse assesses the patient’s comfort using the NRS and finds a score of 7/10. The nurse administers pain medication and provides a warm blanket to improve the patient’s comfort level.
The patient’s NRS score decreases to 3/10, indicating an improvement in comfort.
Future Directions
- Research on the impact of innovative technologies on patient comfort, rest, and sleep (e.g., wearable sensors, sleep tracking devices).
- Development of personalized interventions tailored to individual patient needs and preferences.
- Exploration of the role of mindfulness and meditation in promoting comfort, rest, and sleep.
FAQ Explained
What is the significance of RN Comfort, Rest, and Sleep Assessment?
RN Comfort, Rest, and Sleep Assessment is crucial for identifying and addressing factors that impact patient well-being, recovery, and overall health outcomes.
How do nurses assess patient comfort, rest, and sleep?
Nurses employ various assessment methods, including scales, questionnaires, and direct observation, to evaluate patient comfort, rest, and sleep patterns.
What factors influence patient comfort, rest, and sleep?
Physiological, psychological, environmental, and social factors, such as pain, anxiety, noise, and stress, can significantly affect patient comfort, rest, and sleep.
What nursing interventions can promote patient comfort, rest, and sleep?
Nurses can implement a range of interventions, including pain management, anxiety reduction techniques, environmental modifications, and patient education, to enhance patient comfort, rest, and sleep.
Why is patient education important in promoting comfort, rest, and sleep?
Patient education empowers patients with knowledge and self-care strategies to improve their comfort, rest, and sleep, promoting long-term well-being.